Psoriasis is a relatively common skin ailment and is estimated to affect approximately 8 million people in the United States and about 125 million people worldwide. African Americans have about half the rate of psoriasis as Caucasians. While it is neither contageous nor curable, it is controllable.
Several features of psoriasis are presented in this blog.
Tuesday, March 29, 2011
Pictures of Psoriasis
 |
Psoriasis Vulgaris |
 |
Psoriasis Vulgaris |
 |
Psoriasis Vulgaris |
 |
Psoriasis Vulgaris |
 |
| Psoriasis of the Nails |
 |
Psoriasis Vulgaris |
 |
Psoriasis Vulgaris Erythematous |
 |
Psoriasis Vulgaris Plaque |
 |
Guttate Psoriasis |
 |
Inverse Psoriasis |
 |
Pustular Psoriasis |
 |
Erythrodermic Psoriasis |
 |
Psoriasis of the Scalp |
 |
Psoriatic Arthritis |
Monday, March 28, 2011
Allopathic and Pharmocologic solutions for Psoriasis
Corticosteroids are the most commonly prescribed medicine for psoriasis. They are often used to treat mild to moderate cases and work by reducing inflammation and slowing the growth and build-up of skin cells. They come in creams, ointments, lotions, and foam. Strength is determined by the severity of the area being treated. Steroids can cause side effects, such as thinning of the skin, changes in the skin color, bruising, and dilated blood vessels. Resistance over time may reduce the long-term benefits of steroids.
Dovonex (calcipotriene) is a vitamin D analogue that is sold as a cream, ointment, or solution. It treats psoriasis by slowing down the growth of your skin. It is safer than steroids for long-term use, but Dovonex can irritate the skin and should only be used in small amounts and should not get on the healthy skin surrounding the psoriatic plaques. Dovonex is toxic if ingested, so keep it away from pets and children.
Tazorac (tazarotene) and other retinoids are gels or creams derived from vitamin A. like steriods, retinoids come in different strengths to treat different types of psoriasis in different locations, including the scalp and nails. Tazorac is often combined with steroid treatment. Women who are pregnant or who might become pregnant should probably not use topical retinoids.
Coal tar has been a topical treatment for psoriasis since the nineteenth century. It is sold in many different forms with strengths ranging from 0.5% to 5%. Some preparations may require a prescription. Tar shampoos are often helpful in treating psoriasis of the scalp. Coal tar has a well-deserved reputation for being messy and smelly and can also stain clothing and irritate the skin. However, coal tar products that are on the market now are much easier to use than they once were.
Salicylic acid is used to remove the scales that appear on patches of psoriasis. It is sold in lotions, gels, soaps, and shampoos. Salicylic acid is especially useful in combination with other topical treatments by removing the flakes of dead skin and allowing these other medications to better penetrate the lesions.
When topical treatments begin to fail or the symptoms increase, prescription and non-prescription NSAIDS are at the top of the list of medications used to alleviated the swelling, stiffness and pain of psoriasis. NSAIDS typically do not impact the skin lesions of psoriasis positively. Physicians consider stronger medications when NSAIDS fail and the disease progresses. Common NSAIDS recommended/prescribed for psoriasis include:
Clinoril (sulindac)
Daypro (oxaprozin)
Feldene (piroxicam)
Indocin (indomethacin)
Lodine (etodolac)
Meclomen (meclofenamate)
Mobic (meloxicam)
Motrin, Advil (ibuprofen)
Aleve, Anaprox, Naprelan, Naprosyn (naproxen sodium)
Orudis (ketoprofen)
Relafen (nabumetone)
Tolectin (tolmetin sodium)
Voltaren, Arthrotec (diclofenac)
These medications have significant side effects. The most common side effects of sulindac, piroxicam, meclofenamate, meloxicam, tolmetin sodium and diclofenac involve the gastrointestinal system. They can cause ulcerations of the stomach and small intestine, abdominal pain, cramping, nausea, gastritis, and even serious gastrointestinal bleeding and liver toxicity. Some medications may cause skin rashes.
The most common side effects from oxaprozin, etodolac, ibuprofen, naproxen sodium, ketoprofen are rash, ringing in the ears, headaches, dizziness, drowsiness, abdominal pain, nausea, diarrhea, constipation, heartburn, fluid retention and shortness of breath.
Ibuprofen should be avoided in late pregnancy due to the risk of premature closure of the ductus arteriosus in the fetal heart.
The most common side effects of nabumetone involve the gastrointestinal system. Some studies have shown that nabumetone may have a lower risk of gastrointestinal side effects than the other NSAID medications. However, like other NSAID medications, it still can cause ulcerations, abdominal pain, cramping, nausea, gastritis, and even serious gastrointestinal bleeding, and liver toxicity.
(Side effect information from http://www.medicinenet.com/ Please see same for more detailed side effects.)
When NSAIDS fail, the next line of prescriptions are COX-2 Inhibitors. While these may be less problematic to the stomach, there are other side-effects that include myocardial infarctions, blood clots and stroke, as well as Stevens Johnson Syndrome, a serious allergic skin reaction. Two highly marketed COX-2 inhibitors were removed from the market due to the great rate of serious side effects. VIOXX was removed in 2004 due to increases in heart attacks and strokes; Bextra was removed due to an increased rate of Stevens Johnson Syndrome. Currently Celebrex remains on the market, but its use remains highly controversial.
Disease-modifying antirheumatic drugs or DMARDs may relieve more severe symptoms and may retard or stop the progression of joint and tissue damage. Some common DMARDs include:
- methotrexate (the most widely-used)
- Arava (leflunomide)
- Azulfidine (sulfasalazine)
- Plaquenil (hydroxychloroquine)
- Imuran (azathioprine)
- gold salts
- Sandimmune (cyclosporine)
DMARDs are serious drugs and they can come with serious side effects. Methotrexate users must undergo regular blood tests to check liver and kidney functions.
Leflunomide must not be used during pregnancy because it may cause serious harm (possibly death) to an unborn baby. Women of childbearing age must have a negative pregnancy test before starting this medication and must also use 2 forms of reliable birth control before starting leflunomide, while taking it, and after stopping it until they have finished taking another drug that helps leflunomide leave the body and confirmed through 2 blood tests that the leflunomide levels are very low. Men also must use two effective forms of birth control (e.g., condoms and birth control pills) while taking this medication. It is not known whether this medication affects the sperm. To minimize any possible risk, the manufacturer recommends that men wishing to father a child should consider stopping the medication and using another drug (cholestyramine) as directed to help this drug leave the body before attempting to father a child. This drug may pass into breast milk and could have undesirable effects on a nursing infant. Therefore, breast-feeding is not recommended while using this drug.
Side effects of sulfasalazine include stomach upset, nausea, vomiting, loss of appetite, mouth sores, headache, dizziness, or unusual tiredness may occur. This medication may cause your skin and urine to turn orange-yellow. Temporary male infertility may occur which is reversable when the medication is stopped.
Hydroxychloroquine is an antimalarial that can cause nausea, stomach cramps, loss of appetite, diarrhea, dizziness, or headache may occur. Unlikely but serious side effects may occur: arm/leg/back pain, fast heartbeat, hair loss/color change, mental/mood changes (e.g., anxiety, depression, hallucinations), ringing in the ears/hearing loss, worsening of psoriasis).This medication may infrequently cause serious (sometimes permanent) eye problems or muscle damage, especially if you take it for a long time.
Azathioprine is an immunosuppressant, and as such it suppresses the proliferation of T and B lymphocytes, and reduces the inflammation that accompanies immune reactions and slows damage to the joints caused by the inflammation. The most common serious side effects of azathioprine involve the cells of the blood and gastrointestinal system. Azathioprine can cause serious lowering of the white blood cell count, resulting in an increased risk of infections. This effect is reversed when the dose of azathioprine is reduced or temporarily discontinued. Azathioprine can cause nausea, vomiting, and loss of appetite, which may resolve when the daily dose is reduced or divided and taken more than once a day. Azathioprine can cause liver toxicity and regular testing of blood for blood cell counts and liver functions is required. Other side effects encountered less frequently include fatigue, hair loss, joint pains, and diarrhea.
Biologics are among the newest medications for psoriasis, especially for those who have moderate to severe psoriasis and have not responded favorably to other therapies. Unlike most medications that are chemically synthesized, biologics are derived from natural proteins found in living cells. These medications must be injected because the protein molecules are are too large to be absorbed by the intestine or are too fragile to withstand the stomach acid. Biologics work by inhibiting the immune system, reduces inflammation and inhibit the excessive skin cell growth. Some biologics target T cells and reduce their activity while others reduce the production of TNF. The FDA has approved five for the treatment of plaque and arthritic psoriasis:
Dovonex (calcipotriene) is a vitamin D analogue that is sold as a cream, ointment, or solution. It treats psoriasis by slowing down the growth of your skin. It is safer than steroids for long-term use, but Dovonex can irritate the skin and should only be used in small amounts and should not get on the healthy skin surrounding the psoriatic plaques. Dovonex is toxic if ingested, so keep it away from pets and children.
Tazorac (tazarotene) and other retinoids are gels or creams derived from vitamin A. like steriods, retinoids come in different strengths to treat different types of psoriasis in different locations, including the scalp and nails. Tazorac is often combined with steroid treatment. Women who are pregnant or who might become pregnant should probably not use topical retinoids.
Anthralin (Drithocreme, Micanol) is an effective drug for psoriasis that has been used for almost a century. Originally derived from the bark of the araroba tree, Anthralin works by affecting the growth of skin cells in the patches of psoriasis and reducing inflammation. The advantages of anthralin are that it works well, especially on hard to treat plaques, and it causes no serious side effects. The disadvantages are that it can irritate the skin and stains everything, including clothing, sheets, and even skin. Because of these drawbacks, it's seldom used.
Salicylic acid is used to remove the scales that appear on patches of psoriasis. It is sold in lotions, gels, soaps, and shampoos. Salicylic acid is especially useful in combination with other topical treatments by removing the flakes of dead skin and allowing these other medications to better penetrate the lesions.
When topical treatments begin to fail or the symptoms increase, prescription and non-prescription NSAIDS are at the top of the list of medications used to alleviated the swelling, stiffness and pain of psoriasis. NSAIDS typically do not impact the skin lesions of psoriasis positively. Physicians consider stronger medications when NSAIDS fail and the disease progresses. Common NSAIDS recommended/prescribed for psoriasis include:
These medications have significant side effects. The most common side effects of sulindac, piroxicam, meclofenamate, meloxicam, tolmetin sodium and diclofenac involve the gastrointestinal system. They can cause ulcerations of the stomach and small intestine, abdominal pain, cramping, nausea, gastritis, and even serious gastrointestinal bleeding and liver toxicity. Some medications may cause skin rashes.
The most common side effects from oxaprozin, etodolac, ibuprofen, naproxen sodium, ketoprofen are rash, ringing in the ears, headaches, dizziness, drowsiness, abdominal pain, nausea, diarrhea, constipation, heartburn, fluid retention and shortness of breath.
Ibuprofen should be avoided in late pregnancy due to the risk of premature closure of the ductus arteriosus in the fetal heart.
The most common side effects of nabumetone involve the gastrointestinal system. Some studies have shown that nabumetone may have a lower risk of gastrointestinal side effects than the other NSAID medications. However, like other NSAID medications, it still can cause ulcerations, abdominal pain, cramping, nausea, gastritis, and even serious gastrointestinal bleeding, and liver toxicity.
(Side effect information from http://www.medicinenet.com/ Please see same for more detailed side effects.)
When NSAIDS fail, the next line of prescriptions are COX-2 Inhibitors. While these may be less problematic to the stomach, there are other side-effects that include myocardial infarctions, blood clots and stroke, as well as Stevens Johnson Syndrome, a serious allergic skin reaction. Two highly marketed COX-2 inhibitors were removed from the market due to the great rate of serious side effects. VIOXX was removed in 2004 due to increases in heart attacks and strokes; Bextra was removed due to an increased rate of Stevens Johnson Syndrome. Currently Celebrex remains on the market, but its use remains highly controversial.
Disease-modifying antirheumatic drugs or DMARDs may relieve more severe symptoms and may retard or stop the progression of joint and tissue damage. Some common DMARDs include:
- methotrexate (the most widely-used)
- Arava (leflunomide)
- Azulfidine (sulfasalazine)
- Plaquenil (hydroxychloroquine)
- Imuran (azathioprine)
- gold salts
- Sandimmune (cyclosporine)
DMARDs are serious drugs and they can come with serious side effects. Methotrexate users must undergo regular blood tests to check liver and kidney functions.
Leflunomide must not be used during pregnancy because it may cause serious harm (possibly death) to an unborn baby. Women of childbearing age must have a negative pregnancy test before starting this medication and must also use 2 forms of reliable birth control before starting leflunomide, while taking it, and after stopping it until they have finished taking another drug that helps leflunomide leave the body and confirmed through 2 blood tests that the leflunomide levels are very low. Men also must use two effective forms of birth control (e.g., condoms and birth control pills) while taking this medication. It is not known whether this medication affects the sperm. To minimize any possible risk, the manufacturer recommends that men wishing to father a child should consider stopping the medication and using another drug (cholestyramine) as directed to help this drug leave the body before attempting to father a child. This drug may pass into breast milk and could have undesirable effects on a nursing infant. Therefore, breast-feeding is not recommended while using this drug.
Side effects of sulfasalazine include stomach upset, nausea, vomiting, loss of appetite, mouth sores, headache, dizziness, or unusual tiredness may occur. This medication may cause your skin and urine to turn orange-yellow. Temporary male infertility may occur which is reversable when the medication is stopped.
Hydroxychloroquine is an antimalarial that can cause nausea, stomach cramps, loss of appetite, diarrhea, dizziness, or headache may occur. Unlikely but serious side effects may occur: arm/leg/back pain, fast heartbeat, hair loss/color change, mental/mood changes (e.g., anxiety, depression, hallucinations), ringing in the ears/hearing loss, worsening of psoriasis).This medication may infrequently cause serious (sometimes permanent) eye problems or muscle damage, especially if you take it for a long time.
Azathioprine is an immunosuppressant, and as such it suppresses the proliferation of T and B lymphocytes, and reduces the inflammation that accompanies immune reactions and slows damage to the joints caused by the inflammation. The most common serious side effects of azathioprine involve the cells of the blood and gastrointestinal system. Azathioprine can cause serious lowering of the white blood cell count, resulting in an increased risk of infections. This effect is reversed when the dose of azathioprine is reduced or temporarily discontinued. Azathioprine can cause nausea, vomiting, and loss of appetite, which may resolve when the daily dose is reduced or divided and taken more than once a day. Azathioprine can cause liver toxicity and regular testing of blood for blood cell counts and liver functions is required. Other side effects encountered less frequently include fatigue, hair loss, joint pains, and diarrhea.
Biologics are among the newest medications for psoriasis, especially for those who have moderate to severe psoriasis and have not responded favorably to other therapies. Unlike most medications that are chemically synthesized, biologics are derived from natural proteins found in living cells. These medications must be injected because the protein molecules are are too large to be absorbed by the intestine or are too fragile to withstand the stomach acid. Biologics work by inhibiting the immune system, reduces inflammation and inhibit the excessive skin cell growth. Some biologics target T cells and reduce their activity while others reduce the production of TNF. The FDA has approved five for the treatment of plaque and arthritic psoriasis:
- Enbrel® (etanercept)
- Remicaide® (infliximab)
- Humira® (adalimumab)
- Amevive® (alefacept)
- Remicaide® (infliximab)
- Humira® (adalimumab)
- Amevive® (alefacept)
- Stelara® (ustekinumab)
Systemic medications are prescriptions that work throughout the body, and is an approach that's typically used in moderate to severe cases of psoriasis or psoriasis that hasn't been helped by other topical treatments or phototherapy or that covers more than 10% of the body. Already mentioned are methotrexate and cyclosporine. Other drugs that may be utilized for psoriasis treatment are:
- Acitretin (Soriatane)
- Hydrea (hydroxyurea)
Acitretin is a retinoid derived from Vitamin A. It affects the way skin cells grow and shed. On its own it works well with pustular and erythrodermic psoriasis, but for plaque psoriasis, better results are found in combination with phototherapy. However, this medication causes serious birth defects even after the medication has been stopped. Women should not plan to become pregnant for at least three years after taking Acitretin.
Hydrea is a cancer fighting drug that has shown to be effective against psoriasis and has been used as such for years even though the FDA has not approved it for psoriasis. Women who are pregnant or might become pregnant should not take this medication.
- 6-thioguanine (anti-cancer drug)
- Azulfidine (sulfasalazine) (ulcerative colitis and RA)
- Prograf (tacrolimus) (organ transplant anti-rejection therapy)
- CellCept (mycophenolate mofetil) (organ transplant anti-rejection therapy)
These last four medications are cancer, anti-rejection and GI medications that have shown some positive effects agains psoriasis. While some of these may not be FDA approved for treatment of psoriasis, they have been prescribed off-label for psoriasis management to some degree of success.
PHOTOTHERAPY
Phototherapy may be utilized if topical applications do not improve the condition. Many forms of light therapy can be very beneficial.
Sunlight - generally 20 minutes per day of noon-time sun after gradually increasing exposure from 5 minutes. Too much sun can result in sunburn which can worsen the psoriasis. About 80% of people with psoriasis will notice improvement in their skin from exposure to sunlight.
UVB - This is exposure to the B rays of the sun that penetrate the epidermal layer of the skin. Discovered in 1981, the wavelengths most beneficial to those with psoriasis lie between 300 and 313nm and since then, several companies have developed lanps that operate within a very narrow bandwidth of 311-313nm.
PUVA - This form of treatment is for those who have moderate to severe psoriasis and did not benefit from topical or UVB therapy. This treatment utilizes UVA light (which is a poor treatment by itself) in combination with Psoralen, a chemical derived from plants that makes skin more sensitive to light which is taken orally a few hours prior to treatment or topically via cream or gel about 30 minutes prior to treatment. Protective UVA sunglasses must be worn during treatments and any time the eyes are exposed to sunlight to avoid cataract development, even indoors.
Sunday, March 27, 2011
What Are Symptoms of Psoriasis?
Psoriasis can appear suddenly or slowly. In many cases, psoriasis goes away and then flares up again repeatedly over time.
People with psoriasis have irritated patches of skin. The redness is most often seen on the elbows, knees, and trunk, but it can appear anywhere on the body. For example, there may be flaky patches on the scalp.
The skin patches or dots may be:
Itchy
Dry and covered with silver, flaky skin (scales)
Pink-red in color (like the color of salmon)
Raised and thick
Other symptoms may include:
Genital lesions in males
Joint pain or aching (psoriatic arthritis)
Nail changes, including nail thickening, yellow-brown spots, dents (pits) on the nail surface, and separation of the nail from the base
Severe dandruff on the scalp
Psoriasis may affect any or all parts of the skin. There are five main types of psoriasis:
Erythrodermic -- The skin redness is very intense and covers a large area.
Guttate -- Small, pink-red spots appear on the skin.
Inverse -- Skin redness and irritation occurs in the armpits, groin, and in between overlapping skin.
Plaque -- Thick, red patches of skin are covered by flaky, silver-white scales. This is the most common type of psoriasis.
Pustular -- White blisters are surrounded by red, irritated skin.
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001470/
People with psoriasis have irritated patches of skin. The redness is most often seen on the elbows, knees, and trunk, but it can appear anywhere on the body. For example, there may be flaky patches on the scalp.
The skin patches or dots may be:
Itchy
Dry and covered with silver, flaky skin (scales)
Pink-red in color (like the color of salmon)
Raised and thick
Other symptoms may include:
Genital lesions in males
Joint pain or aching (psoriatic arthritis)
Nail changes, including nail thickening, yellow-brown spots, dents (pits) on the nail surface, and separation of the nail from the base
Severe dandruff on the scalp
Psoriasis may affect any or all parts of the skin. There are five main types of psoriasis:
Erythrodermic -- The skin redness is very intense and covers a large area.
Guttate -- Small, pink-red spots appear on the skin.
Inverse -- Skin redness and irritation occurs in the armpits, groin, and in between overlapping skin.
Plaque -- Thick, red patches of skin are covered by flaky, silver-white scales. This is the most common type of psoriasis.
Pustular -- White blisters are surrounded by red, irritated skin.
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001470/
What Can Cause Psoriasis?
Psoriasis is a very common condition. The disorder may affect people of any age, but it most commonly begins between ages 15 and 35.
The condition cannot be spread to others.
Psoriasis seems to be passed down through families. Doctors think it probably occurs when the body's immune system mistakes healthy cells for dangerous substances. See also: Inflammatory response
Skin cells grow deep in the skin and normally rise to the surface about once a month. In persons with psoriasis, this process is too fast (about 2 weeks instead of 4 weeks) and dead skin cells build up on the skin's surface.
The following may trigger an attack of psoriasis or make the condition more difficult to treat:
Bacteria or viral infections, including strep throat and upper respiratory infections
Dry air or dry skin
Injury to the skin, including cuts, burns, and insect bites
Some medicines, including antimalaria drugs, beta-blockers, and lithium
Stress
Too little sunlight
Too much sunlight (sunburn)
Too much alcohol
In general, psoriasis may be severe in people who have a weakened immune system. This may include persons who have:
AIDS
Autoimmune disorders (such as rheumatoid arthritis)
Cancer chemotherapy
Up to one-third of people with psoriasis may also have arthritis, a condition known as psoriatic arthritis.
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001470/
The condition cannot be spread to others.
Psoriasis seems to be passed down through families. Doctors think it probably occurs when the body's immune system mistakes healthy cells for dangerous substances. See also: Inflammatory response
Skin cells grow deep in the skin and normally rise to the surface about once a month. In persons with psoriasis, this process is too fast (about 2 weeks instead of 4 weeks) and dead skin cells build up on the skin's surface.
The following may trigger an attack of psoriasis or make the condition more difficult to treat:
Bacteria or viral infections, including strep throat and upper respiratory infections
Dry air or dry skin
Injury to the skin, including cuts, burns, and insect bites
Some medicines, including antimalaria drugs, beta-blockers, and lithium
Stress
Too little sunlight
Too much sunlight (sunburn)
Too much alcohol
In general, psoriasis may be severe in people who have a weakened immune system. This may include persons who have:
AIDS
Autoimmune disorders (such as rheumatoid arthritis)
Cancer chemotherapy
Up to one-third of people with psoriasis may also have arthritis, a condition known as psoriatic arthritis.
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001470/
What is Psoriasis??
Psoriasis is a disease that most people think of as primarily a skin disease because the condition causes a persistent rash in various areas of the body. Psoriatic arthritis is a type of joint disease that occurs in roughly seven percent of people who have psoriasis. Psoriatic arthritis affects people of all ages, but most get it between the ages of 30 and 50. Usually a patient has psoriasis (the skin rash) for many years before the arthritis develops, and the arthritis comes on slowly. But this is not always the case. No matter what, patients with psoriatic arthritis must manage both the outbreaks of itchy, scaly skin and the pain and stiffness of arthritis.
http://www.eorthopod.com/content/psoriatic-arthritis
http://www.eorthopod.com/content/psoriatic-arthritis
Saturday, March 26, 2011
OTHER ARTICULAR MANIFESTATIONS IN PSORIATIC ARTHRITIS
Dactylitis
Dactylitis, or sausage digit, is a typical feature of PsA. It refers to infl ammation of the whole digit. It likely
results from both synovitis in the joints of the digit, as well as tenosynovitis, particularly in the fl exor tendons.
Dactylitis most commonly affects the toes, but fingers are affected as well.
It should be noted that dactylitis may become chronic, such that it is no longer painful or red, but remains as a chronically swollen digit, which may not respond to therapeutic intervention.
Dactylitis http://www.cdaarthritis.com/images_slides/43_spon2_d_adactylitisfinger_720.jpg
Tenosynovitis
Tendonitis or tenosynovitis occurs frequently among patients with PsA. Infl ammation may affect the fl exortendons of the fingers, as well as the extensor carpi ulnaris, sites that are commonly affected in RA. Achillestendonitis is commonly seen, as is plantar fascitis. These may interfere with function and may lead to disability. In PsA, tendonitis may be associated with tendon nodules and signifi cant functional limitation.
Enthesitis
Infl ammation of the enthesis, site of insertion of tendoninto bone, is another typical feature of PsA. Enthesitis
may occur at any tendon insertion site, but most commonlyaffects the plantar fascia, Achilles tendon insertion,
insertion of tendons at the knee and shoulder, aswell as the pelvic bones. It has been suggested thatenthesitis alone in the presence of psoriasis may be sufficient for the diagnosis of PsA.
Other Extra-Articular
Manifestations
Iritis is an extra-articular feature common to all spondyloarthropathies and is also seen among patients with
PsA. Some 7% of patients with PsA present with iritis,and it can also be seen among patients with psoriasis
without arthritis.
Urethritis is also a feature of seronegative disease. It
is less common in PsA than in the other members of the
spondyloarthritis group.
Bowel involvement may occur in patients with PsA
and is usually nonspecifi c colitis.
Cardiac abnormalities have been reported among
patients with PsA, including dilatation of the base of
the aortic arch which occurs in ankylosing spondylitis.
More recently it has been recognized that patients
with PsA are at risk for cardiovascular disease.
This may be related to the metabolic abnormalities
associated with PsA, including hyperlipidemia, hyperuricemia,
as well as lifestyle factors such as obesity and
smoking.
X-Ray Findings in Psoriatic Arthritis
The general features and diagnostic signs of psoriatic arthritis include: asymmetric distribution, soft tissue swelling, normal bone mineralization, erosions, fluffy periostitis, and a narrowed or widened joint space.
In the hands, psoriatic arthritis is usually asymmetric. A ray pattern is usually seen in the DIP joints. Mouse ears sign, pencil in cup deformity, and opera glass hand deformity are also radiographic signs of psoriatic arthritis in the hands and feet. Joint space widening is common due to fibrous tissue deposition and bone destruction.
The sacroiliac joints are involved in up to 50% of patients with psoriatic arthritis. The distribution is usually bilateral, but asymmetric and the joint space is narrowed.
Psoriatic arthritis in the spine is most common in the upper lumbar and lower thoracic area. There is a presence of marginal and non-marginal syndesmophytes, with the latter being the most common. It is usually asymmetric and unilateral.
*All information gathered from Yochum and Rowe's Essentials of Skeletal Radiology - 3rd Edition.
In the hands, psoriatic arthritis is usually asymmetric. A ray pattern is usually seen in the DIP joints. Mouse ears sign, pencil in cup deformity, and opera glass hand deformity are also radiographic signs of psoriatic arthritis in the hands and feet. Joint space widening is common due to fibrous tissue deposition and bone destruction.
The sacroiliac joints are involved in up to 50% of patients with psoriatic arthritis. The distribution is usually bilateral, but asymmetric and the joint space is narrowed.
Psoriatic arthritis in the spine is most common in the upper lumbar and lower thoracic area. There is a presence of marginal and non-marginal syndesmophytes, with the latter being the most common. It is usually asymmetric and unilateral.
*All information gathered from Yochum and Rowe's Essentials of Skeletal Radiology - 3rd Edition.

Anteroposterior radiograph of the hands shows subchondral erosions of the fourth left distal interphalangeal joint and right third and fourth proximal interphalangeal joints with periosteal reaction. Courtesy of Bruce M. Rothschild, MD

Anteroposterior radiograph of the feet shows arthritis mutilans. Courtesy of Bruce M. Rothschild, MD.

Anteroposterior radiograph of the thumb shows arthritis mutilans. Courtesy of Bruce M. Rothschild, MD.

Anteroposterior radiograph of the pelvis in a male patient shows sacroiliitis in association with psoriasis. Courtesy of Ali Nawaz Khan, MBBS.
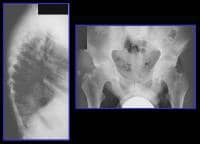
Left, lateral radiograph of the dorsal spine of a 38-year-old man shows spondylitis in association with psoriasis. Note the squaring of the anterior vertebral bodies. Right, radiograph of the pelvis in the same patient shows sacroiliitis and erosive changes around both hip joints. Courtesy of Ali Nawaz Khan, MBBS.
X-Ray Finding in Psoriatic Arthritis
There are five different types of psoriatic arthritis which include:

- Arthritis mainly in the small digits of the fingers or toes (55-70%)
- Asymmetrical arthritis in the joints of the extremities (30-50%)
- Symmectrical polyarthritis which can look like rheumatoid arthritis (15-70%)
- Arthritis mutilans: this is very rare, but can be very destructive to the joints (3-5%)
- Arthritis in the sacroiliac joints and the spine (5-33%)

Posteroanterior radiograph of the hands shows wrist fusion. Courtesy of Bruce M. Rothschild, MD.
X-Ray Finding in Psoriatic Arthritis
Twenty-three percent of people with arthritis have psoriatic arthritis. Psoriatic arthritis usually occurs in people 30-50 years old, and usually about 10 years after the first signs of psoriasis occur. It is very rare to develop psoriatic arthritis without first having psoriaris.


Anteroposterior radiograph of the abdomen shows fusion of the sacroiliac joints. Courtesy of Bruce M. Rothschild, MD.
Therapeutic approach to Psoriasis
The following has been shown to help psoriatic patients: decreasing sugar, meat, animal fats, and alcohol; increase dietary fiber, and cold water fish, have a healthy B.M.I.; eliminate gluten and any other potential food alergies.
Supplements shown to help the psoriatic patient include: multi-vitamin, mineral formula, flaxseed oil, vitamin A, Vitamin D, Vitamin E, Chromium, selenium, zinc.
Botanical Medicines that may be useful include: Goldenseal, smilax sarsparilla , and milk thistle
Reducing stress levels have been shown to help psoraitic patients.
Justin Felsman
Supplements shown to help the psoriatic patient include: multi-vitamin, mineral formula, flaxseed oil, vitamin A, Vitamin D, Vitamin E, Chromium, selenium, zinc.
Botanical Medicines that may be useful include: Goldenseal, smilax sarsparilla , and milk thistle
Reducing stress levels have been shown to help psoraitic patients.
Justin Felsman
Individual Nutrients
- Increase vitamin A and zinc
- Increase chromium due to psoriatics have increased serum insulin and glucose
- Increase selenium and vitamin E intake to decrease Glutathione peroxidase
- Increase oral 1 alpaha (OH) D3.
- potentially utilize oral dimethyl fumaric acid or topical monoethethyl if natural therapies fail. The acid has side effects such as flushing of skin, nausea, diarrhea, malaise, gastric pain, mild liver and kidney disfunction.
How Nutrition can help the psoriatic patient
Fish oil at 10-12 grams and 1.2 grams of docosahexaenoic acid has been shown to improve symptoms.
Wild cold- water fish (salmon, mackerel,or hering) plus 1 tbsp flaxseed oil daily may be advantageous because of the lipid peroxidases in many fish oil products.
EPA(eicosapentaenoic acid) improves psoriasis because of competitiion for arachidonic acid binding sites, inhibiting synthesis of inflamatory leukotrienes from arachodonic acid, which are elevated up to 800 times in psoriatic patients compared to non-psoriatic patients. A tissue-intrinsic unidentified inhibitor of cyclooxygenase is involved.
Cyclooxegenase inhibitors (asprin, nsaids) may exacerbate psoriasis. Lipoxygenase inhibitors(benoxyaprofen) may improve psoriasis. Natural substances ( quercetin, ubiquitous plant flavonoid), vitamin E, onion, and garlic inhibit lipoxygenase.
Arachadonic acid is found in animal fats and dairy so these substances should be limited. Psoriasis is also linked to body mass index and inversely related to intake of carrots, tomatoes, fresh fruits, and index of beta- arotene intake. Fasting and vegetarian regimens help psoriatics, probably because of decreased gut-derived toxins and polyamines. Gluten-free and elimination diets are beneficial. Justin Felsman
Wild cold- water fish (salmon, mackerel,or hering) plus 1 tbsp flaxseed oil daily may be advantageous because of the lipid peroxidases in many fish oil products.
EPA(eicosapentaenoic acid) improves psoriasis because of competitiion for arachidonic acid binding sites, inhibiting synthesis of inflamatory leukotrienes from arachodonic acid, which are elevated up to 800 times in psoriatic patients compared to non-psoriatic patients. A tissue-intrinsic unidentified inhibitor of cyclooxygenase is involved.
Cyclooxegenase inhibitors (asprin, nsaids) may exacerbate psoriasis. Lipoxygenase inhibitors(benoxyaprofen) may improve psoriasis. Natural substances ( quercetin, ubiquitous plant flavonoid), vitamin E, onion, and garlic inhibit lipoxygenase.
Arachadonic acid is found in animal fats and dairy so these substances should be limited. Psoriasis is also linked to body mass index and inversely related to intake of carrots, tomatoes, fresh fruits, and index of beta- arotene intake. Fasting and vegetarian regimens help psoriatics, probably because of decreased gut-derived toxins and polyamines. Gluten-free and elimination diets are beneficial. Justin Felsman
Tuesday, March 22, 2011
Other Cool Blogs To Check Out
http://www.westonaprice.org/blogs/kdaniel/
http://www.westonaprice.org/blogs/cmasterjohn/
http://www.psoriasis-aid.com/
http://www.westonaprice.org/blogs/cmasterjohn/
http://www.psoriasis-aid.com/
Subscribe to:
Posts (Atom)

